|
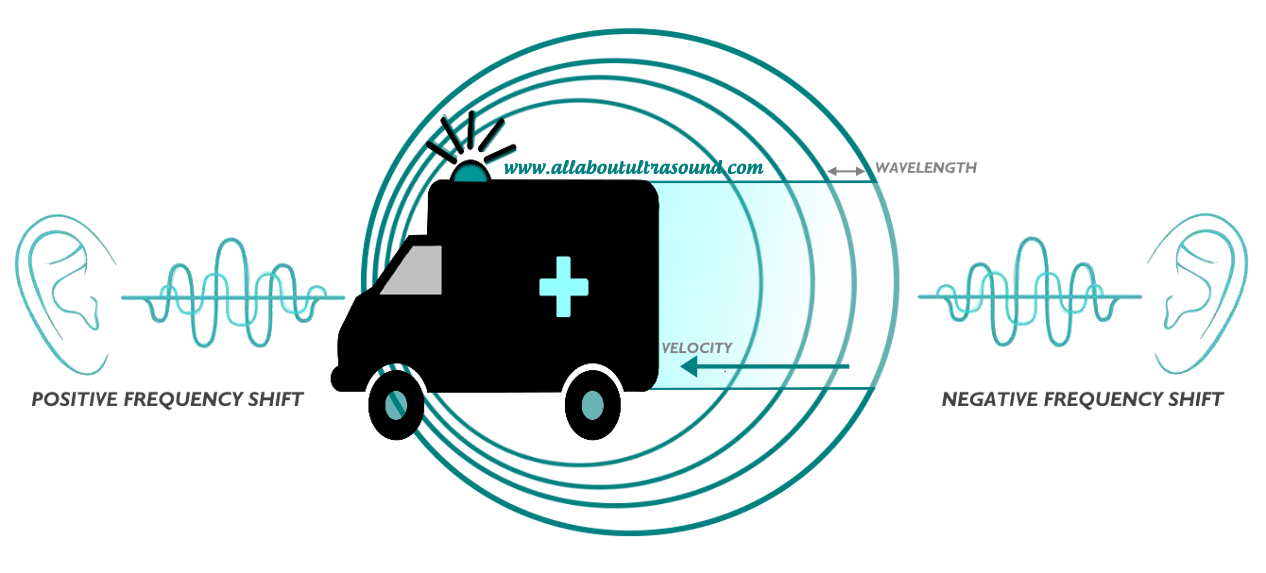
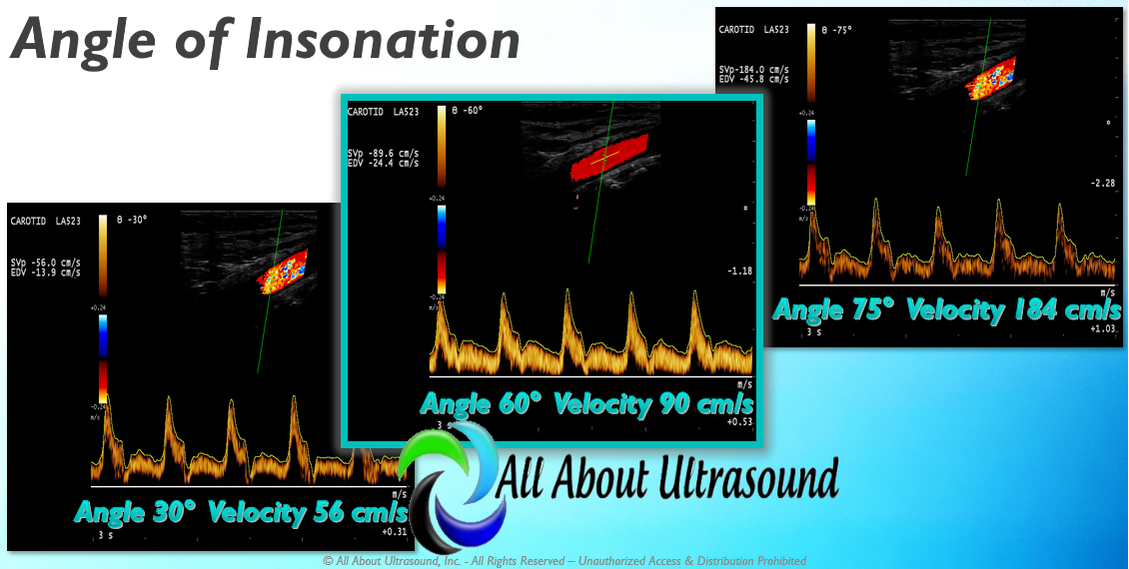
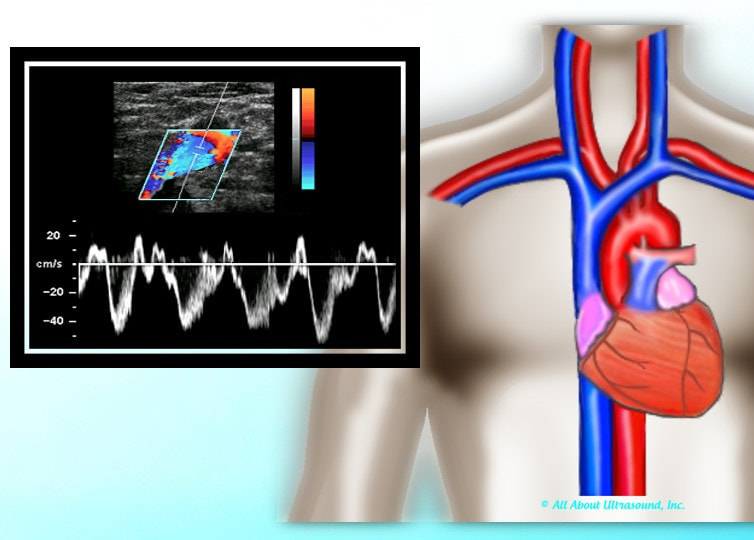
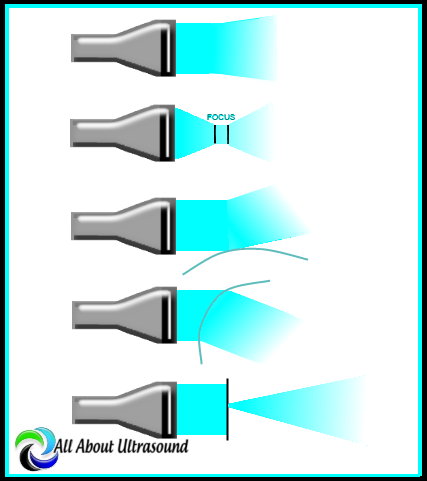
It is so easy to get caught up with our patients who need our immediate attention for things that aren't even ultrasound related and even seasoned sonographers can ignore physics altogether, but when we take it back to the basics, this is where image optimization begins. So, let's take a step back and look at the basics again..... Doppler principles and hemodynamics... I know, I know, for some just saying the words brings tears to their eyes as they recall sleepless nights studying for the Ultrasound Physics registry! But no need to fear! Doppler is simple when you break it down. So the Doppler Effect is quite simply either a positive shift which is a compression in the wavelength (a higher frequency) or a negative shift, which results in an elongated wavelength, (a lower frequency) and this is of course all relative to the observer. So what does this have to do with Doppler ultrasound? I'm glad you asked. Doppler frequency shifts come from moving red blood cells and give us the spectral display that we see in Continuous Wave and Pulse Wave Doppler. The velocities obtained from these frequency shifts can also be displayed in Color Doppler, superimposed on top of the 2D ultrasound image. This is a method of displaying the mean or average velocity, while the spectral Doppler display can quantify specific velocities, like the peak systolic and end diastolic velocities, at a point in time. Because the Doppler frequency shift is relative to the position of the observer, this is important when placing the Doppler sample and angle of insonation. The Doppler sample volume is the "observer" and the frequency shift created by the moving red blood cell is what we are evaluating on the spectral display. But what happens if the observer changes position? The velocity observed will be different. This is extremely important for Doppler Angle. The Society for Vascular Ultrasound recommends that scanning angle be maintained between 45-60 degrees. While we know that the closer to 0 degrees, the more accurate the velocity result because of the math and the cosine of the angle, try getting that on a your average carotid Doppler. It is often not attainable and so for reporting and to maintain consistency in the lab, it is best to stay within the range of what can be easily obtained on most exams. So as you can see from the image, as the angle of insonation is moved, the velocity result is SIGNIFICANTLY impacted. This can be a very big factor in following up serial ultrasound studies if the same Doppler angle is not used for follow up exams. This is why it is so important to look at the previous study images, especially if there is disease. So when you're scanning don't forget these very basic settings and factors that can have a large impact on your patient's results. Studying for your SPI ULTRASOUND PHYSICS REGISTRY? We have you covered with our SPI Ultrasound Physics Registry Review course and FREE TRIAL available! Want more info on Doppler Principles and Hemodynamics? Need CME's? See our Mastering Doppler Principles and Hemodynamics E-Learning CME Course! Approved for 1 SDMS CME Credit Hour
5 Comments
Master the concepts of Upper Extremity Duplex, including Hemodialysis Access and More! Our new CME Opportunity with E-Learning On Demand. This E-Learning course has been approved for 2 SDMS CME Credit Hours. Register today! CLICK HERE
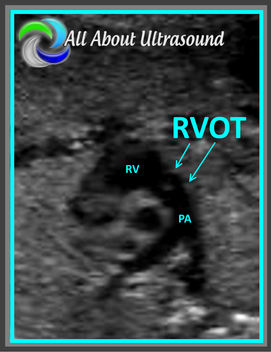
It is application time again for the ARDMS® Pediatric Echo Registry. The next time to apply is January 3, 2018-March 6, 2018. Apply for your registry and study with us today! Our Pediatric Echo Ultrasound Registry Review Quiz starts at just $19.99 and can help you prepare for that dreaded registry exam. No need to be intimidated. With over 200 questions in our unlimited quiz, our Test & Learn format will help you learn as you go, testing your knowledge and teaching too! Our test responses are based on your answers and questions are designed to help you learn as you go. Don't be overwhelmed by ultrasound physics or any other ultrasound specialty registry exam.... we have the tools to help you master the content and pass your ARDMS/CCI registries. Simple. Easy. Done!
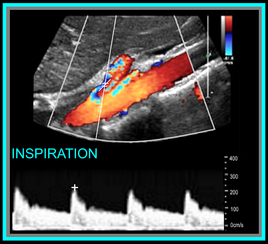
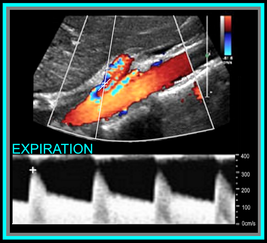
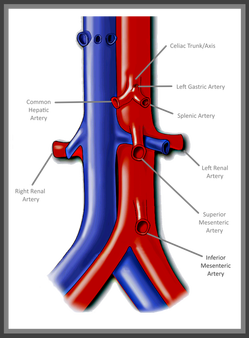 Mesenteric Abdominal Duplex – it sounds complicated right? In reality though, as long as your patient is prepped, there’s not much to it. I say that with caution though – we’ve all had those patients that just really need another modality of testing. Let's be real... we all know that our ultrasound transducer is NOT a magic wand! First and foremost - Patient Prep! Your patient prep is one of the most important factors when performing Mesenteric Duplex Ultrasound. Your patient needs to be NPO for at least 6-8 hours before scanning. A test done without the right prep, might as well have not been done at all. This is for a number of reasons: 1. You can't see squat with air and gas in the way! 2. The mesenteric arterial system should be scanned both pre and post prandial for evaluation of stenosis and arterial ischemic response. 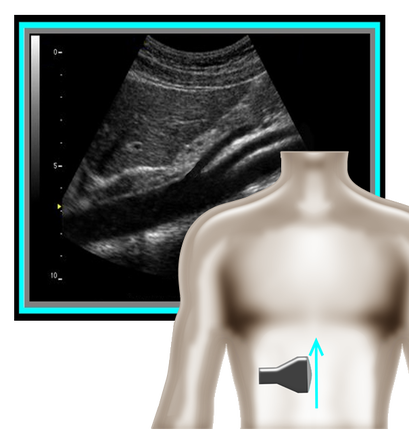 So where to begin and what protocol? I've got that covered for you! A mesenteric duplex protocol should include, at a minimum... Transverse and Longitudinal approach with 2D, Longitudinal approach with Color and PW Doppler (Record PSV and EDV) at each of the following locations: •Proximal Aorta •Celiac Artery/Trunk •Branching of Common Hepatic Artery and Splenic Artery from the Celiac Artery •SMA origin, proximal, mid, distal •IMA origin, proximal and as distal as possible •IVC A few things can help you improve your imaging and will also help you evaluate patient pathology.
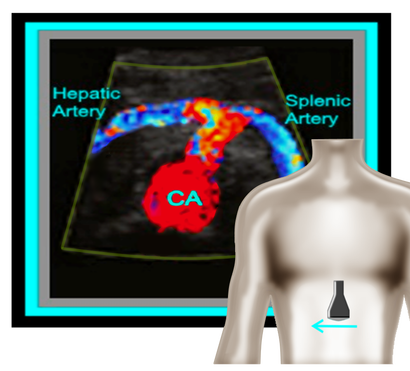 Okay, so now that we have the basics out of the way... you're probably wondering, what should the waveforms look like and what is normal/abnormal? So here's a quick guide: Celiac Artery Remember that the Celiac Artery supplies the liver, spleen and stomach, which are low resistance vascular beds. Normal Doppler waveforms will show increased diastolic flow because of the organs supplied. Flow may also increase with inspiration. Don't forget to evaluate the branches! This is best done in a transverse plane. ≥70% Celiac Artery Stenosis will show a peak systolic velocity of ≥200 cm/s. 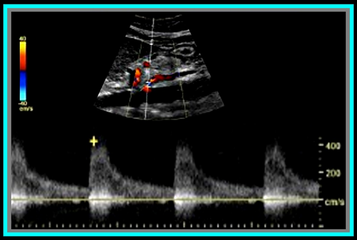 Superior Mesenteric Artery Remember that the SMA supplies the jejunum, ileum, and both the right and transverse colon. Because of this, waveform characteristics will vary based on state (ie. NPO, post-prandial). Diastolic flow will increase as needed for digestion, post-prandially. In the normal vessel, post-prandial evaluation should show increased peak systolic flow velocities. If PSV flow does not increase, this is suggestive of a hemodynamically significant stenosis. Also keep in mind that inspiration will show an increase in peak systolic velocities. ≥70% SMA stenosis will show a peak systolic velocity of ≥275cm/s or absence of color flow in the SMA. End diastolic flow velocities of ≥45cm/s are also an indication of ≥70% SMA stenosis. Also keep in mind that you can find pathology based on the angle of the SMA takeoff from the aorta. If the angle is markedly increased, it may indicate the presence of adenopathy. The SMA should course parallel to the aorta. Inferior Mesenteric Artery The IMA supplies the distal 1/3 of the transverse colon, splenic flexure, descending colon, sigmoid colon and rectum. It's waveform characteristics are similar to the SMA and will vary based on state (ie. NPO, post-prandial). Diastolic flow will increase as needed for digestion, post-prandially. ≥70% IMA stenosis will show a peak systolic velocity of ≥275cm/s or absence of color flow in the IMA. You may need to get your magic wand out for this one! Diagnostic Criteria Reference: Moneta, et al GET OUR FREE SCANNING TIPS QUICK GUIDE
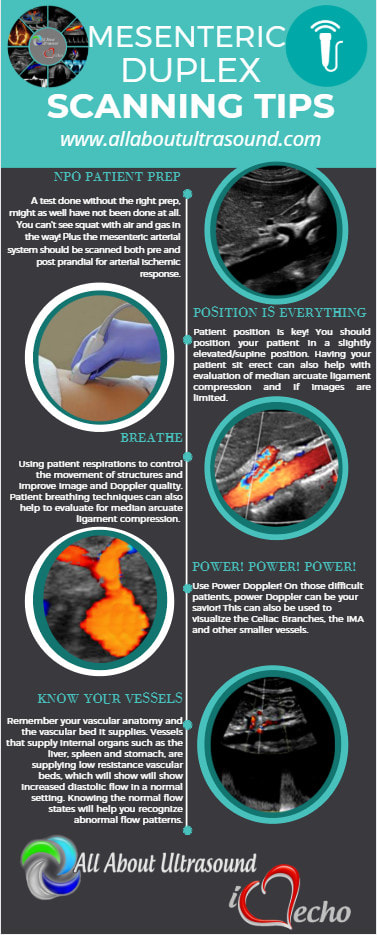
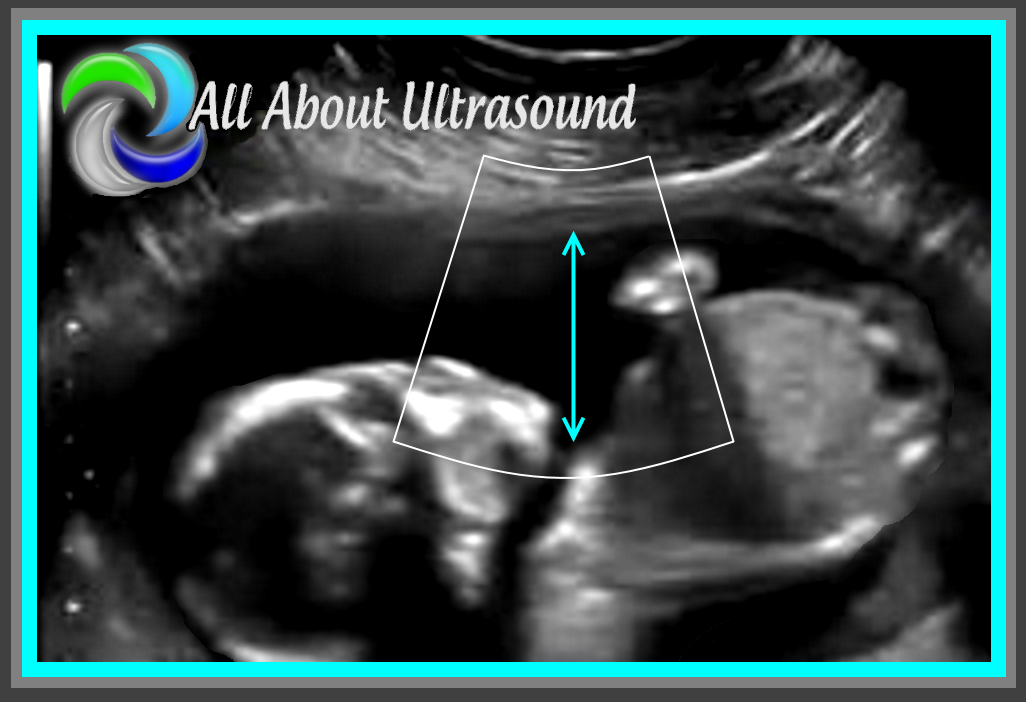
 2. Scanning and trying to find those ovaries can prove to be a challenge with a pregnant uterus! Even though it is not our focus, we can’t forget those ovaries! Making sure to image those along with the uterus and fetal images will ensure that you’re not missing potential pathology, but it can definitely be tough with that pregnant uterus in the way. Best methods are to bring the transducer laterally to the patient’s side and to scan in a transverse plane along the lateral side of the uterus, starting pretty high up and moving down toward the patient’s cervix. That transverse plane will give you an increased field of view and will allow you to identify structures more easily.
Don't miss our next LIVE SCANNING Event! In Sunny, Fort Lauderdale - July 15th 8:30am-12:30pm.
Together with the professionals from CardioServ, LLC we are hosting this amazing opportunity to learn venous insufficiency ultrasound. This course is for sonographers and physicians interested in learning correct techniques for performing and interpreting venous reflux.
Unlike many other imaging modalities, scanning ultrasound is completely dependent on the sonographer, the angle of the probe and small little adjustments made to the machine settings. So often, it can be easy to just take that picture and move along. At All About Ultrasound, we want to make sure that sonographers like you have all the tools, tips, techniques and resources to not just pass a test or take a picture, but to excel at what you do. We want to give you the tools you need to transition from being a picture taker to being a critical thinker and an investigator. An image protocol is great for making sure that your images meet the basic standard criteria for accreditation and the basics of performing an exam, but it shouldn't end there. How do you investigate and give the physician what they need to make a diagnosis? How do you as the sonographer make a difference in the outcome of your patient? How do you learn and grow your skillset?
While we do offer many resources to add to your learning, we know that only those sonographers who truly seek out education and apply what they learn will ultimately be able to relate this back investigative patient care. So, don't forget that there is a purpose for what you do. There is a reason you became a sonographer - the reason is your patient. Don't get so caught up in following the protocol that you don't ever go beyond it to investigate and piece the puzzle together to answer the clinical questions. You are not a picture taker - you are the eyes of the physician and without your investigative ultrasound skills, that doctor may not have what they need to treat the patient. So don't ever forget to seek out the answer, ask the questions, take that extra picture, take that extra Doppler sample and put that amazing sonographer brain to work. You are the eyes, the ears and the hands that can make a difference. It is so easy to get caught up in the day-to-day routine, but don't forget your WHY! Answer the age old question |
Details
Making Waves™All About Ultrasound presents Making Waves™, our ultrasound specific blog and newsletter. Join us here for ultrasound news, cases and more! Don't FORGET YOUR MERCH!Archives
May 2023
Categories
All
|







 RSS Feed
RSS Feed