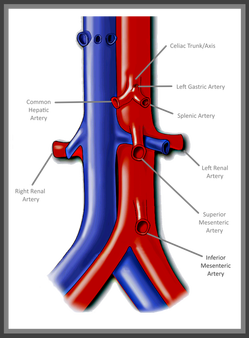
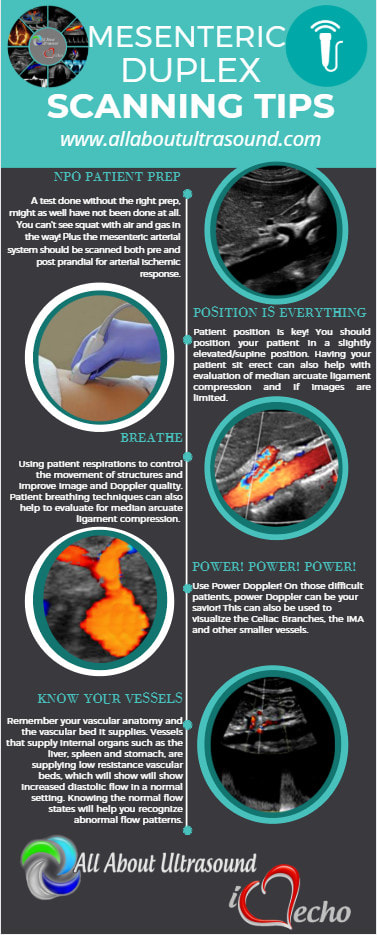
 Mesenteric Abdominal Duplex – it sounds complicated right? In reality though, as long as your patient is prepped, there’s not much to it. I say that with caution though – we’ve all had those patients that just really need another modality of testing. Let's be real... we all know that our ultrasound transducer is NOT a magic wand! First and foremost - Patient Prep! Your patient prep is one of the most important factors when performing Mesenteric Duplex Ultrasound. Your patient needs to be NPO for at least 6-8 hours before scanning. A test done without the right prep, might as well have not been done at all. This is for a number of reasons: 1. You can't see squat with air and gas in the way! 2. The mesenteric arterial system should be scanned both pre and post prandial for evaluation of stenosis and arterial ischemic response. 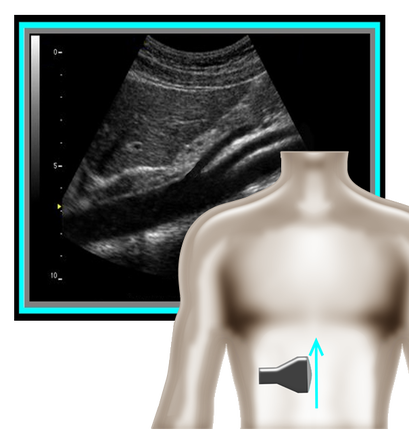 So where to begin and what protocol? I've got that covered for you! A mesenteric duplex protocol should include, at a minimum... Transverse and Longitudinal approach with 2D, Longitudinal approach with Color and PW Doppler (Record PSV and EDV) at each of the following locations: •Proximal Aorta •Celiac Artery/Trunk •Branching of Common Hepatic Artery and Splenic Artery from the Celiac Artery •SMA origin, proximal, mid, distal •IMA origin, proximal and as distal as possible •IVC A few things can help you improve your imaging and will also help you evaluate patient pathology.
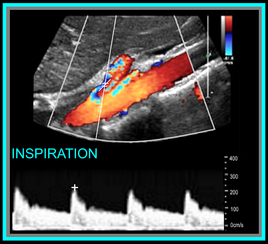
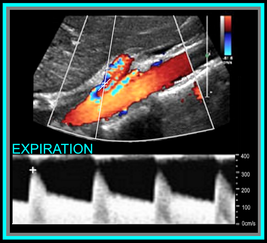
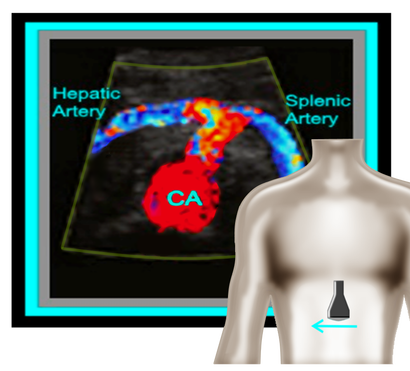 Okay, so now that we have the basics out of the way... you're probably wondering, what should the waveforms look like and what is normal/abnormal? So here's a quick guide: Celiac Artery Remember that the Celiac Artery supplies the liver, spleen and stomach, which are low resistance vascular beds. Normal Doppler waveforms will show increased diastolic flow because of the organs supplied. Flow may also increase with inspiration. Don't forget to evaluate the branches! This is best done in a transverse plane. ≥70% Celiac Artery Stenosis will show a peak systolic velocity of ≥200 cm/s. 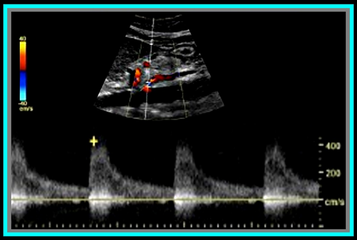 Superior Mesenteric Artery Remember that the SMA supplies the jejunum, ileum, and both the right and transverse colon. Because of this, waveform characteristics will vary based on state (ie. NPO, post-prandial). Diastolic flow will increase as needed for digestion, post-prandially. In the normal vessel, post-prandial evaluation should show increased peak systolic flow velocities. If PSV flow does not increase, this is suggestive of a hemodynamically significant stenosis. Also keep in mind that inspiration will show an increase in peak systolic velocities. ≥70% SMA stenosis will show a peak systolic velocity of ≥275cm/s or absence of color flow in the SMA. End diastolic flow velocities of ≥45cm/s are also an indication of ≥70% SMA stenosis. Also keep in mind that you can find pathology based on the angle of the SMA takeoff from the aorta. If the angle is markedly increased, it may indicate the presence of adenopathy. The SMA should course parallel to the aorta. Inferior Mesenteric Artery The IMA supplies the distal 1/3 of the transverse colon, splenic flexure, descending colon, sigmoid colon and rectum. It's waveform characteristics are similar to the SMA and will vary based on state (ie. NPO, post-prandial). Diastolic flow will increase as needed for digestion, post-prandially. ≥70% IMA stenosis will show a peak systolic velocity of ≥275cm/s or absence of color flow in the IMA. You may need to get your magic wand out for this one! Diagnostic Criteria Reference: Moneta, et al GET OUR FREE SCANNING TIPS QUICK GUIDE
6 Comments
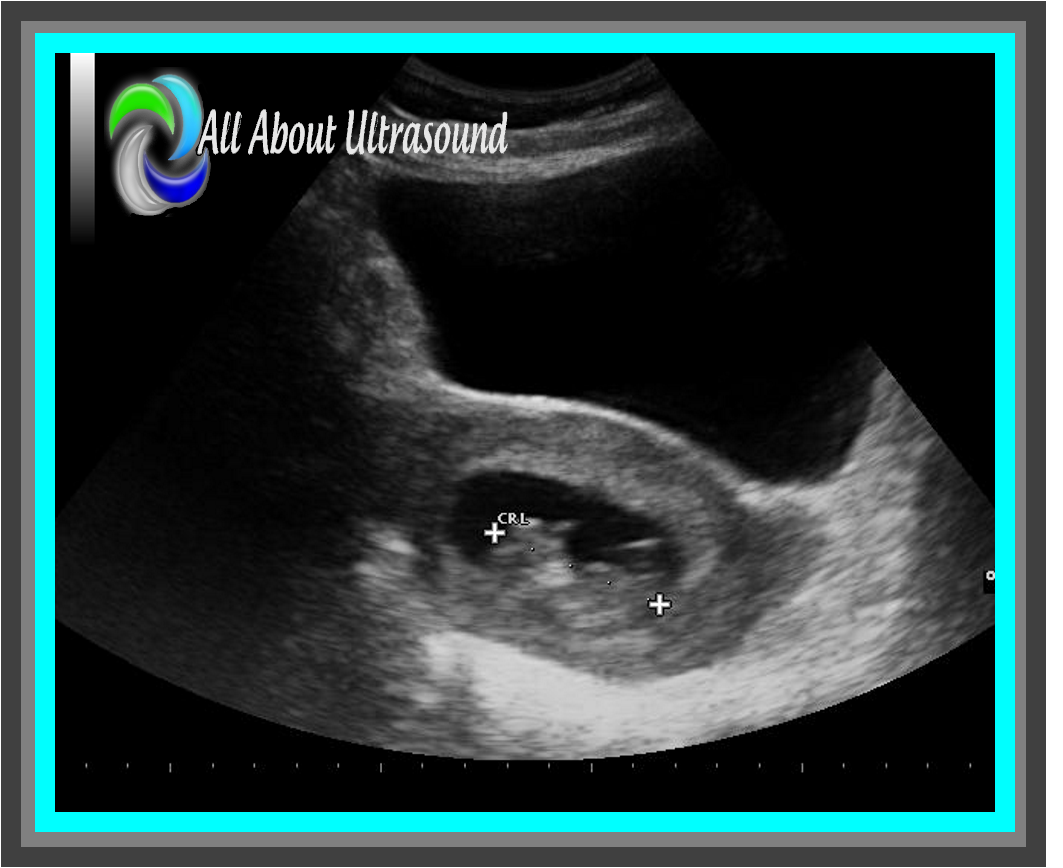
 2. Scanning and trying to find those ovaries can prove to be a challenge with a pregnant uterus! Even though it is not our focus, we can’t forget those ovaries! Making sure to image those along with the uterus and fetal images will ensure that you’re not missing potential pathology, but it can definitely be tough with that pregnant uterus in the way. Best methods are to bring the transducer laterally to the patient’s side and to scan in a transverse plane along the lateral side of the uterus, starting pretty high up and moving down toward the patient’s cervix. That transverse plane will give you an increased field of view and will allow you to identify structures more easily.
|
Details
Making Waves™All About Ultrasound presents Making Waves™, our ultrasound specific blog and newsletter. Join us here for ultrasound news, cases and more! Don't FORGET YOUR MERCH!Archives
May 2023
Categories
All
|





 RSS Feed
RSS Feed